By the Global X ETF research team
The COVID-19 pandemic has shed light on systemic inefficiencies in the healthcare space and proven that the value of remote medicine goes far beyond a short-term solution during a global pandemic. At the core of its adoption lays an emerging policy framework that extends current Medicare telehealth reimbursement and prescribing waivers beyond the COVID-19 Public Health Emergency (PHE).
We believe the economic and social benefits of telemedicine are creating an environment where the technology will be ingrained across healthcare verticals. In this piece, we highlight different ways industry players are gearing up for the long-term adoption of telemedicine and virtual care offerings.
Key Takeaways
- Recent federal legislation and policy proposals look to ensure telemedicine is accessible long after the pandemic ends.
- Amid policy coverage uncertainty, telemedicine and digital health firms are tailoring their solutions to meet patient needs and facilitate the right balance between in-person care and virtual care.
- The digital health industry is building a foundation for increasingly connected services, including pharmacy fulfillment and diagnostic capabilities, that we expect to increase the industry’s value proposition.
Telemedicine Finds Policy Support Beyond the Pandemic
In response to COVID-19, state and federal governments enacted short-term measures to facilitate the use of telemedicine. These measures allowed for Centers for Medicare & Medicaid Services (CMS) coverage of telehealth services, allowed practitioners to prescribe controlled substances to patients using telemedicine. We also saw physician licensing requirements ease, allowing physicians to treat patients via telemedicine across state lines.1Largely due to these short-term policies, telehealth use is now 38 times higher than pre-pandemic levels.2
Now that patients and providers have seen that better, more efficient healthcare exists, many are pushing for permanent solutions to the restrictive pre-existing regulations.3 To that end, we’ve seen multiple recent efforts:
- Citing expand access to care, reduced costs, and improved health outcomes, a bipartisan group of 47 senators called for the extension of expanded coverage to telehealth services to be included in must-pass legislation in February.4
- A recent letter, signed by over 300 organizations, urged Congress to establish “a pathway to comprehensive telehealth reform.” Amazon, Teladoc, Walmart, Zocdoc, and Zoom are among the firms calling for change.5
Given increasing pressure, Congress recently introduced the Telehealth Extension and Evaluation Act, bipartisan legislation that looks to extend current Medicare telehealth reimbursement and prescribing waivers for two years after the COVID-19 PHE. The bill would also allow for a study on the impact of telehealth services on Medicare beneficiaries to inform future legislation.6
Payment Parity at the Heart of the Discussion
Though long-term regulations easing the use of telehealth have bipartisan support, there is debate about how exactly to implement them. At the heart of the discussion is payment parity, which would require insurers to reimburse telehealth and in-person services at the same rate.7
There are a few factors informing the logic behind payment parity and the circumstances in which it would be appropriate. In some instances, for example, telemedicine is not an appropriate option for patients as it cannot ensure the same level of care.8 Certain patient interactions, for instance, require a thorough in-person examination to develop a diagnostic or treatment plan. On the flip side, sweeping legislation limiting payment parity could disincentivize physicians from using telemedicine as they would receive less revenue per consultation.9 (See: Telemedicine & Digital Health Are Crossing the Chasm for more detail on how telemedicine fits value-based priorities set by CMS).
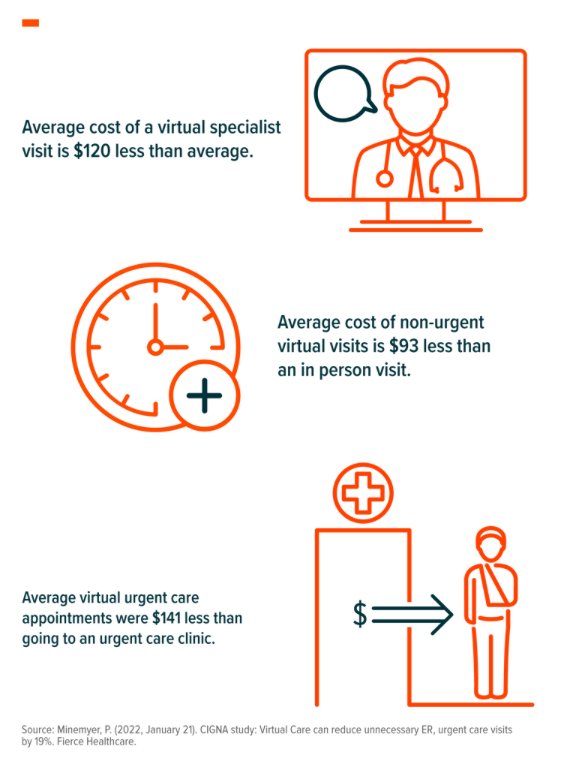
While Congress figures out the specifics of long-term telehealth legislation, private insurers recognize the value of remote and digital care and are moving swiftly to make telemedicine accessible to their customers for the long term. Anthem, UnitedHealthcare, Cigna, and CVS Health’s Aetna all now offer employers virtual primary care plans.10 Cigna, via their recently acquired telemedicine platform MDLive, conducted a study to measure the impact of accessible telemedicine. They report that patients who saw virtual providers also saw 19% fewer visits to the ER or urgent care. Study participants also saw steep discounts vs in-person care:11
Telemedicine Offers Patients and Providers Flexibility
In our view, the firms best-positioned for growth will be able to strike and communicate the right balance between virtual and in-person care. We believe the three major subsegments of telehealth – virtual primary care, virtual chronic care, and virtual mental health – are poised for significant growth as industry leaders tailor their services to these specific use cases.
- Virtual Primary Care encompasses day-to-day healthcare provided by a licensed professional. Services include family medicine, general internal medicine, general pediatrics, and obstetrics and gynecology.12 When appropriate, the provider coordinates with specialists and offers a hybrid approach of telemedicine and in-person care.13 As the virtual primary care segment gets increasingly more competitive, players would be well served to find ways to differentiate themselves. Most recently, Amazon and Teladoc, via a recent partnership, are offering Amazon Alexa-enabled audio consultations for non-emergent visits.14 Anthem, on the other hand, is leveraging AI-backed modeling and data analytics to build out each patient’s personalized care plan.15
- Virtual Chronic Care Management entails continuous care to patients living with chronic conditions like diabetes, congestive heart failure, and chronic obstructive pulmonary disease (COPD). CMS reports that 93% of overall Medicare spending comes from two-thirds of Medicare beneficiaries with multiple chronic.16 Virtual chronic care management, currently more than any other telehealth subsegment, offers a unique opportunity to leverage remote patient monitoring. The advent of new technology to remotely measure vitals and automatically report them to a physician will be key in offering more comprehensive care to patients. To fully engrain the use of digital health, the industry should look to mimic the success diabetes monitoring has seen, where medication is automatically dispensed to the patient when vitals are deemed outside of normal range.
- Virtual Mental Health is the fastest-growing subsegment of telemedicine. It currently makes up 40% of Teladoc’s annual revenue, and the firm estimates a 30-40% compound annual growth rate (CAGR) through 2024.17 About 11% of the global population, an estimated 800 million people worldwide, live with a mental health condition.18 As the space continues to grow and gain acceptance, we expect players that focus on clinical evidence that demonstrates the benefits of virtual mental health to differentiate themselves from the competition. Consolidation across mental health segments is also expected, to provide a hub of services that encompasses therapy, psychiatric care, and meditation, among others.
To read this post in its entirety, click here and visit the Global X ETF blog.
Photo Credit: Gamaliel Cabana via Flickr Creative Commons
FOOTNOTES
1. Telehealth.HHS.gov. (n.d.). Policy changes during COVID-19. Retrieved February 28, 2022.
2. Bestsennyy, O., Gilbert, G., Harris, A., & Rost, J. (2021, July 9). Telehealth: A quarter-trillion-dollar post-COVID-19 reality? McKinsey & Company.
3. King, R. (2022, February 8). Senators to craft major mental health package with focus on reforming pay parity, expanding telehealth. Fierce Healthcare.
4. U.S. Senator for Hawai’i Brian Schatz. (2022, January 28). Schatz, Wicker lead group of 45 lawmakers in calling for extension of pandemic telehealth expansion [Press release].
5. American Telemedicine Association. (2022, January 31). Re: Establishing a pathway for comprehensive telehealth reform.
6. Landi, H. (2022, February 8). Senators introduce bipartisan bill to extend patient access to telehealth through 2024. Fierce Healthcare.
7. Center for Connected Health Policy. (2022, January 19). Private payer: parity – federal.
8. Ellimoottil, C. (2021, May 10). Understanding the case for telehealth payment parity. Health Affairs – Health Affairs Forefront.
9. Baumann, B. C., MacArthur, K. M., & Michalski, J. M. (2020, September 2). The importance of temporary telehealth parity laws to improve public health during COVID-19 and future pandemics. International Journal of Radiation, Oncology, Biology, Physics, 108(2), 362-363. https://doi.org/10.1016/j.ijrobp.2020.05.039
10 Palmer, A., & Coombs, B. (2022, February 9). Amazon rolls out its telehealth service nationwide. CNBC.
11. Minemyer, P. (2022, January 21). Cigna study: Virtual Care can reduce unnecessary ER, urgent care visits by 19%. Fierce Healthcare.
12. Institute of Medicine (US) Committee on the Future of Primary Care. (1996). Defining primary care. In M.S. Donaldson, K. D. Yordy, K. N. Lohr, & N. A. Vanselow (Eds.), Primary Care: America’s Health in a New Era (pp. 27-51). National Academies Press.
13. Gliadkovskaya, A. (2022, January 20). How 24/7 remote cardiac monitoring can cut diagnosis time, according to one tech company. Fierce Healthcare.
14. Wetsman, N. (2022, February 28). Telehealth visits now available through Amazon Alexa. The Verge.
15. Minemyer, P. (2022, February 8). Anthem rolling out virtual primary care to plans in 11 states. Fierce Healthcare.
16. Comfort, A. (2021, November 3). The future of virtual chronic care management. Population Health Learning Network: First Report – Managed Care.
17. Teledoc Health, LLC. (2021, November 18). 2021 Investor Day [PowerPoint slides]. Teledoc Health’s News & Events.
18. Auxier, B., Bucaille, A., & Westcott, K. (2021, December 1). Mental health goes mobile: The mental health app market will keep on growing. Deloitte Insights.
19. Bingham, J. M., Black, M., Anderson, E. J, Li, Y., Toselli, N., Fox, S., Martin, J. R., Axon, D. R., & Silva-Almodóvar, A. (2020, August 20). Impact of telehealth interventions on medication adherence for patients with type 2 diabetes, hypertension, and/or dyslipidemia: A systematic review. The Annals of Pharmacotherapy, 55(5), 637-649. https://doi.org/10.1177/1060028020950726
20. Kim, J., Combs, K., Downs, J., & Tillman III, F. (2018, January 19). Medication adherence: The elephant in the room. U.S. Pharmacist, 43(1), 30-34.
21. Lohuis, P. (n.d.). 6 tips for improving medication adherence with telehealth. Health Recovery Solutions.
22. 23andMe. (2021, November 1). 23andMe announces the closing of its acquisition of Lemonaid Health [Press release].
23. Torrence, R. (2021, October 22). Microsoft integrates healthcare cloud service with Cerner EHR for smoother telehealth visits. Fierce Healthcare.
DISCLOSURE
Investing involves risk, including the possible loss of principal. The Health Care and Information Technology sectors can be affected by government regulations, rapid product obsolescence, intense industry competition and loss or impairment of patents or intellectual property rights. International investments may involve risk of capital loss from unfavorable fluctuation in currency values, from differences in generally accepted accounting principles or from social, economic or political instability in other nations.